By GEOFF MULVIHILL
Nebraska will change into the primary state to implement new work necessities for some folks with Medicaid medical health insurance underneath a legislation President Donald Trump signed final 12 months.
Gov. Jim Pillen, a Republican, introduced Wednesday that the requirement would take impact within the state Might 1 and will affect about 30,000 individuals who have barely larger incomes than conventional Medicaid beneficiaries.
“We’re not right here to take all people to the curb,” he mentioned. As a substitute, he mentioned, the intention is “ensuring we get each able-bodied Nebraskan to be a part of our neighborhood.”
The sweeping tax and coverage legislation Trump signed in July requires states to ensure many recipients are working by 2027 however gave them the choice to do it sooner.
Beneficiaries could have extra reporting duties
The legislation mandates that folks ages 19 to 64 who’ve Medicaid protection work or carry out neighborhood service at the very least 80 hours a month or be enrolled in class at the very least half-time to obtain and maintain protection.
It applies solely to individuals who obtain Medicaid protection by means of an growth that covers a inhabitants with a barely larger revenue restrict. Forty states and the District of Columbia have opted to develop the protection revenue tips underneath former President Barrack Obama’s 2010 medical health insurance overhaul.
Of 346,000 Nebraska residents enrolled in Medicaid as of Might, about 72,000 had been within the larger revenue growth group.
Some folks shall be exempted, together with disabled veterans, pregnant ladies, dad and mom and guardians of dependent youngsters underneath 14 or disabled people, individuals who had been just lately launched from incarceration, those that are homeless and folks getting habit remedy. States may also provide short-term hardships for others in the event that they select.
All Medicaid beneficiaries who’re eligible due to the growth shall be required to submit paperwork at the very least each six months exhibiting they meet the mandate.
Those that don’t would lose their protection.
The reporting requirement is twice as frequent as it’s for most individuals lined by Medicaid now. That change means extra work for the state companies — and for a few of them, in depth and sure costly pc program updates.
Pillen mentioned he doesn’t anticipate the state authorities to extend staffing to make the adjustments.
When and the best way to implement the change is more likely to be on the agenda for governors and state lawmakers throughout the nation as legislative classes begin — most of them in January.
The coverage is anticipated to result in misplaced protection
The nonpartisan Congressional Funds Workplace estimates that the requirement will cut back Medicaid prices by $326 billion over a decade — and that it’ll end in 4.5 million folks changing into uninsured annually beginning in 2027. Presently, about 77 million Individuals are lined by Medicaid.
As a result of most individuals lined by Medicaid who’re in a position to work already do, it’s not anticipated to extend employment charges.
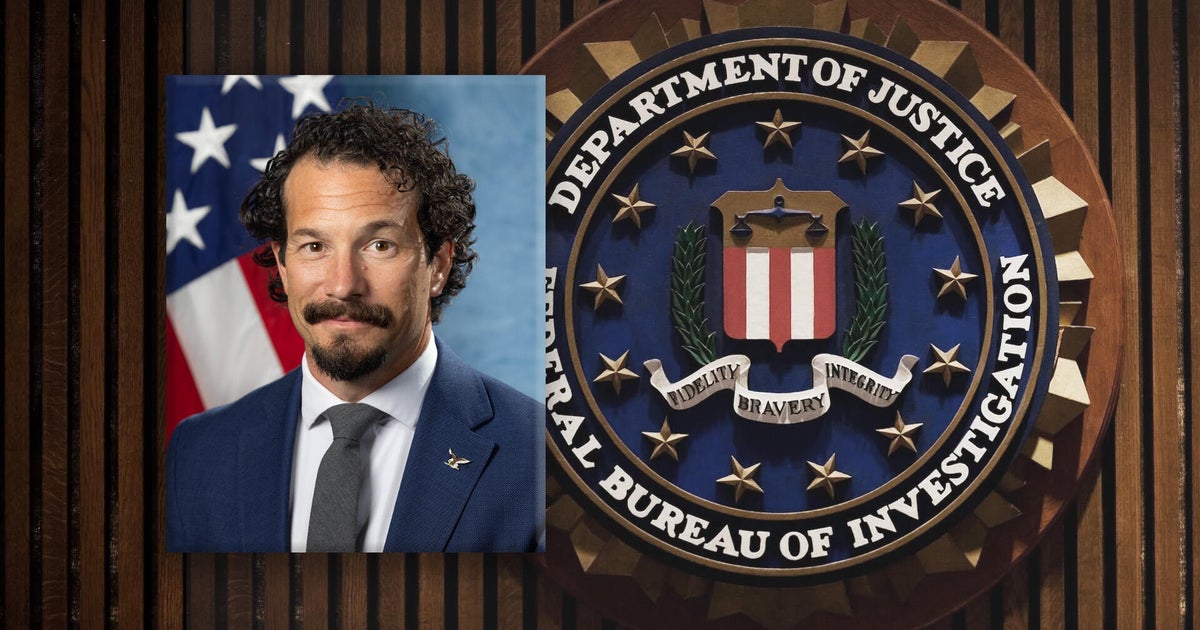
Mehmet Oz, the administrator of the Facilities of Medicare and Medicaid Companies, joined Pillen’s announcement through a video feed and mentioned the administration believes there are jobs obtainable throughout the nation, and the problem is connecting folks with them.
“Most people who find themselves able-bodied on Medicaid truly need to get a job,” Oz mentioned.
Georgia applied comparable necessities in 2023. Far fewer individuals are lined than projected, partly due to the work and reporting necessities.
Arkansas tried one other variation of Medicaid work necessities — later blocked by a choose — that noticed 18,000 folks kicked off protection within the first seven months after it took impact in 2018.